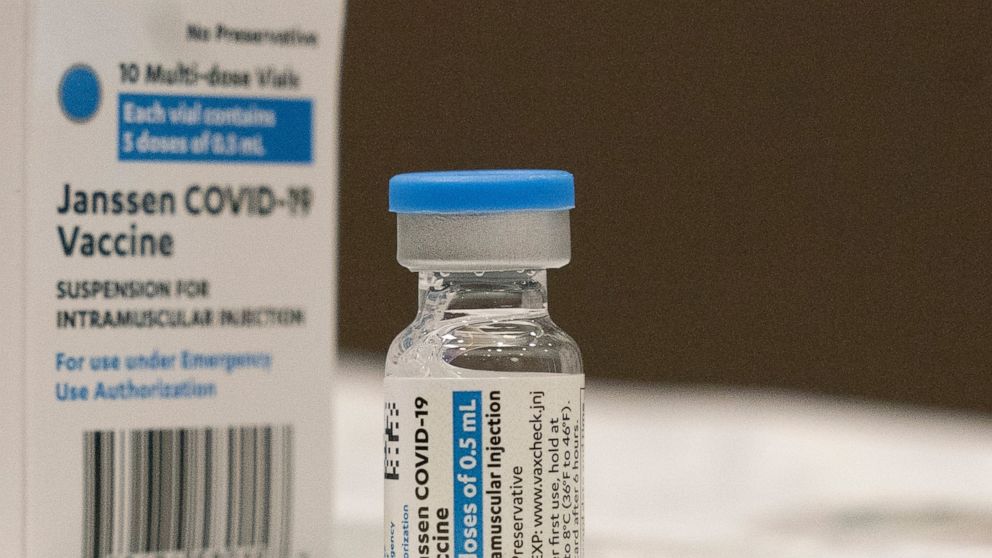
FDA panel takes up tough questions on J&J COVID-19 boosters
U.S. health advisers are meeting to tackle who needs boosters of Johnson & Johnson’s single-shot COVID-19 vaccine and when
WASHINGTON — U.S. health advisers on Friday tackled who should get boosters of Johnson & Johnson’s single-shot COVID-19 vaccine and when — and whether using a competing brand for the second dose might provide better protection.
The push for boosters kicked off last month after the Food and Drug Administration authorized third doses of the Pfizer vaccine for seniors and younger adults with health problems, jobs or living conditions that place them at higher risk from the coronavirus. On Thursday, an FDA advisory panel unanimously recommended a half-dose booster of the similar Moderna vaccine for the same groups.
Friday, the same panel discussed a booster of J&J’s vaccine but the decision is more complex. Moderna and Pfizer asked the FDA to OK boosters at least six months after immunization, but J&J proposed a sliding schedule with an extra dose as early as two months later.
Adding another twist, the experts also will discuss preliminary data from a government “mix-and-match” study that suggested J&J recipients may have a far stronger immune response if they get either a Moderna or Pfizer booster rather than a second J&J dose.
The FDA will use its advisers’ recommendations to decide whether to authorize boosters for both J&J and Moderna, likely next week, after which another government agency will rule on who should roll up their sleeves.
All three vaccines in the U.S. still offer strong protection against severe illness and death from COVID-19 — and the nation’s priority remains getting first doses to 66 million eligible but unvaccinated Americans who are most at risk as the extra-contagious delta variant continues to circulate.
But experts continue to debate whether there’s value in using boosters to head off milder infections in most vaccinated adults, an approach proposed by the Biden administration.
J&J’s single-shot vaccine is made with a different technology than the two-shot Pfizer and Moderna vaccines — and it has consistently shown lower effectiveness levels. But the company argued Friday that there’s little sign of that effectiveness waning over eight months, citing 70% protection against symptomatic COVID-19 in the U.S.
And a large study found that giving a second dose just two months after the first bumped that protection up to 94%. Giving that booster six months later instead prompted an even bigger jump in virus-fighting antibodies. But the company has tested a six-month booster in far fewer people, prompting concern from FDA’s scientists.
“I’m not seeing the rationale for waiting” since a rapid second dose was so potent, said FDA adviser Dr. Hayley Gans of Stanford University.
Timing flexibility is important because “there are perhaps some populations that might benefit more than others” from an extra dose sooner and others could wait, said J&J’s Dr. Johan Van Hoof.
In their own review, FDA scientists flagged a number of shortcomings with J&J’s booster studies, including only a tiny portion of cases involving the delta variant, by far the dominant strain in the U.S. Reviewers also warned that J&J had only followed booster recipients for a little more than a month after a second dose, making it hard to draw conclusions about the durability of protection. Finally, FDA staff emphasized that they had not had time to independently confirm J&J’s findings, which were submitted shortly before the meeting.
FDA’s reviewers found no new safety concerns after a second J&J dose, but again, they cautioned about the small number of patients studied and short follow-up period.
The J&J vaccine was highly anticipated for its one-and-done formulation. But its rollout earlier this year was hurt by a series of troubles including manufacturing problems and some rare but serious side effects including a blood clot disorder and a neurological reaction called Guillain-Barre syndrome. In both cases, regulators decided the shot’s benefits outweighed those risks.
The vast majority of the 188 million Americans who are fully vaccinated against COVID-19 have received the Pfizer or Moderna options, while J&J recipients account for only about 15 million.
———
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.
![]()