Preliminary study results suggest the drug Trump touted doesn’t work for very sick coronavirus patients
“I think from the review that I heard basically it was not seen as a positive, not seen as a negative,” Cuomo said during CNN’s coronavirus town hall.
The study, sponsored by the New York state Department of Health, looked at about 600 patients at 22 hospitals in the greater New York City area.
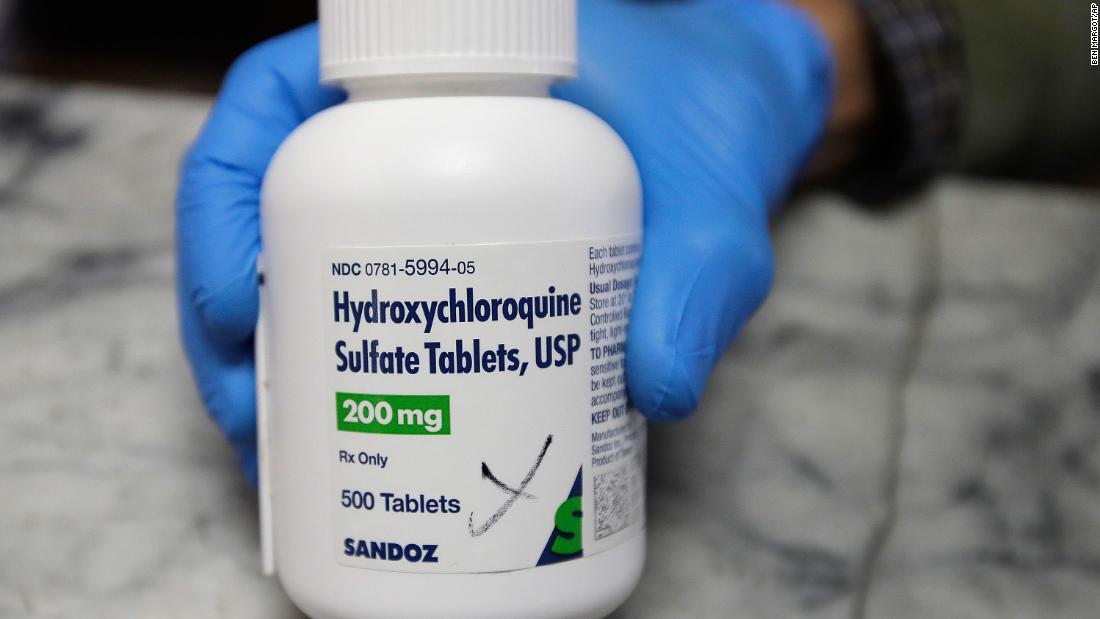
Those who took hydroxychloroquine, with or without the antibiotic azithromycin, were no more likely to survive their infections than those who did not, according to David Holtgrave, dean of the University at Albany School of Public Health, who conducted the study. The results have not yet been peer-reviewed or published.
“We don’t see a statistically significant difference between patients who took the drugs and those who did not,” he said.
Since hydroxychloroquine and azithromycin are both already on the market for other illnesses, doctors are free to prescribe them to coronavirus patients if they want to, and the Albany study found that doctors did often use them to treat their coronavirus patients.
Dr. William Schaffner, a Vanderbilt University infectious disease expert who was not involved in the Albany report, said while it’s hardly the last word on the issue, he hopes it will guide doctors who are considering prescribing it to their hospitalized patients.
“This study is not a red light. It’s a yellow caution light,” he said.
In the Albany study, patients who were taking hydroxychloroquine were also not statistically more likely to develop heart problems, a known side effect of the drug. Doctors in Brazil, France, and Sweden have found that coronavirus patients taking the drug did have a higher rate of developing cardiac complications.
Hydroxychloroquine has shown promise against the virus in the lab, and doctors theorized it would also tamp down inflammation, which can cause serious complications for people with Covid-19.
The author of the Albany report said he hopes his study adds to the general knowledge about the usefulness of these drugs against coronavirus, given that doctors are using it already.
“Hopefully what we’ve done here is to start collecting data and evidence and learning lessons as we go forward about effects and side effects,” Holtgrave said he expects the final results of his research to be released as soon as next week and it will include 1,200 patients.
Holtgrave emphasized that this is just one study, and that more significant studies — those that look at the drugs as part of a clinical trial — still have not reported their results. The Albany study is observational, meaning that the researchers looked back at people who had already been prescribed the drugs.
During CNN’s town hall, FDA Commissioner Dr. Stephen Hahn called the Albany research a significant observational study.
“Obviously you need to wait for the entire cohort of individuals to have been treated with the complete course of treatment to get a full read on that,” he said.
The final Albany report will also include information about whether patients taking the drugs were more or less likely to be admitted to the intensive care unit, or to have a longer or shorter stay in the hospital, as well as death rates for each group.
Trump has been a cheerleader for hydroxychloroquine
Hydroxychloroquine, a decades-old drug used to treat malaria, lupus and rheumatoid arthritis, became a political football last month when President Trump said it showed “tremendous promise” against Covid-19.
“I think it’s going to be great,” he said.
He’s also made the drug sound like it was harmless, when in fact it can have potentially deadly side effects. Earlier this month he said if people take the drug, it can “help them, it’s not going to hurt them” and that he was considering taking it himself.
The University at Albany study included some 600 patients: about 300 took the combination of hydroxychloroquine and azithromycin; some 200 took one of the two drugs; and approximately 100 took neither drug and served as a control group for comparison.
The Albany researchers found doctors were more likely to prescribe the drugs to patients who were already very sick. For example, the patients who were prescribed the drugs were more likely to have underlying diabetes and coronary disease, and they were also more likely to have shortness of breath upon admission to the hospital.
Since the patients who took the drugs were more ill to start with, they did have higher rates of death and heart complications. However, once the researchers did a statistical adjustment, they found no statistically significant difference in the death or complication rates between the patients who took the drugs and those that didn’t.
Holtgrave said while it looks like the drugs did not work for very sick patients, researchers should consider studying whether they would work to treat patients who are mildly ill, or possibly as prevention from getting sick in the first place.
“Our study could inform the direction and design of other randomized trials,” he said.
More studies needed
The observational trial done at Albany has inherent issues.
“You never know what the biases were that persuaded physicians to use the drug in some patients rather than others and these biases often cannot be measured,” Schaffner said.
A different kind of study, called a double-blind randomized clinical trial, is considered the gold standard in medicine. Such trials, now ongoing, involve a large group of Covid-19 patients randomly assigned to take the drug or a placebo, which is a pill that has no effect. Neither the patients nor the doctors know who’s getting the drugs and who’s getting the placebo.
There are more than two dozen clinical trials of hydroxychloroquine going on in the US right now, according to clinicaltrials.gov, a government database. It will take weeks to months to get results.
Schaffner emphasized that those trials should continue. Vanderbilt is one of the centers conducting the trials, although Schaffner is not involved.
“We know what the limitations of observational studies are, and so I look forward to the results of the prospective control trials,” he said.
CNN’s Devon Sayers, Wes Bruer and Dr. Minali Nigam contributed to this report.
![]()